Oral Surgery, Dental Implants & Wisdom Teeth Removal in Southern California
By the time they are in their forties, more than half of individuals will have lost at least one tooth due to an oral condition or an accident. Dental implants will fill in any gaps in your smile and make it look great again if you have any missing teeth. Simply said, dental implants are prosthetic teeth that we can surgically place in your mouth. They will blend in with your other teeth and set in your jaw permanently. With the right maintenance, your implants might last a lifetime and improve how you look and eat.
Dentures, which have evolved through time but still have drawbacks, can be considered as an alternative to dental implants. To keep dentures in place, messy adhesive must be applied. When you’re eating or talking, they could still move around or even fall out. They also need to be cleaned and cared for frequently. Nonetheless, dental implants are permanent after they are placed, and taking care of them is very similar to taking care of your natural teeth.
Just about anyone with healthy gums and adequate bone structure in their mouth is a good candidate for dental implants.

Wisdom Teeth
All of a person’s permanent teeth should have fully emerged by the time they turn 12 or 13. The final four molars, or wisdom teeth, are the outliers since they typically don’t begin to “erupt” from under the gums until early adulthood. Unfortunately, wisdom teeth frequently erupt unevenly. They may come out at strange angles, brush up against neighboring teeth, or even get stuck in the jawbone. The issue is that many people’s bites aren’t large enough to accommodate additional space for new molars, and when a wisdom teeth can’t erupt normally, it gets impacted. This may result in severe health issues such dental decay, nerve damage, tooth pain, infection, and crooked teeth.
Impacted wisdom teeth and the issues they cause can be difficult to predict in advance, and later in life, surgical removal might be challenging. Because of this, doctors frequently advise young patients to have their wisdom teeth extracted as a preventative step. The removal of wisdom teeth is a frequent outpatient treatment that OC Smile completes in-house. You will need to rest and abstain from specific foods after the first 24 hours, but you’ll find that recovery happens rather quickly. The process is straightforward and will assist you in avoiding numerous tooth issues down the road.
What to expect during your procedure
X-rays are frequently taken prior to your oral surgery to help with diagnostic and treatment planning. You should feel free to ask any questions you may have. The procedure will be described in detail, along with your available anaesthetic alternatives. Your recuperation process will be influenced by the surgery you are having and your general health. It’s always vital to inform your healthcare providers about the prescription and over-the-counter medications you use, any ongoing medical issues you may have, and if you smoke. Your safety and comfort—always the top priorities—will be helped by this.
Fullerton, CA Oral Surgery Dental Office – Best Oral Surgeon Near Me - Wisdom Teeth Removal in Mission Viejo, CA
 Sinus Lift Near Me
Sinus Lift Near Me
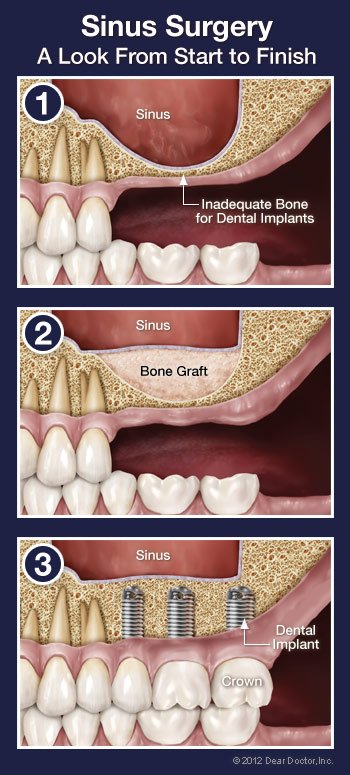
If you want a state-of-the-art dental implant to replace a lost or failing tooth, your dentist will need to make sure you have enough bone in your jaw to secure the implant. This is true regardless of the type of tooth that needs to be replaced. However, if the implant is for an upper back tooth and there isn’t enough bone under the gum where it has to go, the implant’s base may wind up pushing through a sinus cavity (an air space to the side of the nose). This is a concern since you can’t anchor a dental implant to air, but it’s one that can usually be rectified with a little in-office surgical procedure called a “sinus membrane lift.”
A sinus membrane lift, or sinus augmentation, involves adding bone to fill in the bottom of that air space, essentially raising the floor of the sinus cavity. Why wouldn’t there be enough bone there already? For some people, it’s simply a matter of how large their sinus cavities are, and their shape. In other cases, bone has actually been lost from the area. If your tooth has been missing for a long period, the bone that once surrounded it may have started to degrade. Bone, in general, need stimulation to stay strong, and the teeth provide such stimulation to the jawbone. The bone loses stimulation when teeth are gone, and the body stops producing new bone cells in that area. As a result, bone volume and density are reduced. In addition, if your tooth loss was caused by periodontal (gum) disease, the condition may have caused your tooth-supporting bone to deteriorate. A sinus membrane lift can build more bone where it is needed, no matter what the cause of deficient bone is.
Where does this additional bone come from? It could be bone from another portion of your body, such as your hip or another part of your jaw. However, the most common materials treated in a laboratory for these purposes are bone grafting materials. It’s possible that the original source was a human or animal donor (usually a cow). It is also possible to employ synthetic products. The Food and Drug Administration must approve all grafting materials, and they must be manufactured according to their requirements. The materials are sterilized, non-contagious, and devoid of rejection factors thanks to an unique treatment. Bone grafts, for the most part, serve as scaffolds that the body eventually replaces with its own bone.
The Sinus Lift Procedure
Your dentist will use x-ray imaging to analyze the form, position, and condition of your sinuses before scheduling surgery. Your anesthetic options will also be explored. The operation is normally performed under local anesthetic, which involves numbing the region, much like a routine filling. Some people need extra sedation or anti-anxiety medicine, which can be given orally (by mouth) or intravenously (via a vein) through injection.
An incision will be made in your gum to expose the bone that used to contain your missing tooth or teeth once the area has been totally numbed. The membrane that lines the sinus will be shown through a small incision in the bone. The membrane will be lifted, and the cavity beneath it filled with bone grafting material. After that, the gum is sewn back together. In some circumstances, the implant(s) can be inserted directly into the grafting material before the gums are closed, avoiding the need for a second surgical treatment later. However, the surgical site is frequently let to heal for 6-7 months before an implant is inserted.
What to Expect After Sinus Surgery
An incision will be made in your gum to expose the bone that used to contain your missing tooth or teeth once the area has been totally numbed. The membrane that lines the sinus will be shown through a small incision in the bone. The membrane will be lifted, and the cavity beneath it filled with bone grafting material. After that, the gum is sewn back together. In some circumstances, the implant(s) can be inserted directly into the grafting material before the gums are closed, avoiding the need for a second surgical treatment later. However, the surgical site is frequently let to heal for 6-7 months before an implant is inserted.
 Oral Cancer Screening in Spokane Valley
Oral Cancer Screening in Spokane Valley
Oral cancer may not receive as much attention as other cancers with a larger public profile, but that doesn’t make it any less deadly. Oral cancer is expected to kill one person per hour, every day in the United States. Oral cancer is deadly since it isn’t frequently identified until it has progressed to an advanced stage, despite the fact that it accounts for a small percentage of all malignancies. The chances aren’t good at that point: just around 6 out of 10 persons will survive five years of treatment.
Would you take a simple test that could give you an early indication of whether you’re likely to develop this disease? There is, in fact, good news! This test can genuinely save lives because early detection has been demonstrated to enhance the survival probability of oral cancer to 80% or better. And, best of all, an oral cancer screening is included in a routine dental visit that you should be getting anyway.
Oral cancer screening is quick and painless. Its goal is to find subtle changes in the mouth, lips, and tongue lining tissues that could indicate the early stages of this type of cancer. The primary focus of the screening is a visual and tactile (touch) evaluation. If any anomalies are discovered, a tiny tissue sample might be taken for laboratory examination.
Who’s At Risk for Developing Oral Cancer?
You might be surprised by the response. Oral cancer was once assumed to be a disease of the elderly, and it still primarily affects people over the age of 40. Younger people, on the other hand, are now the fastest-growing segment of mouth cancer patients. The spread of the sexually transmitted Human Papilloma Virus is mostly to blame.
The other important risk factors, of course, remain: Oral cancer is more likely to occur if you’re middle-aged or older, a moderate to heavy drinker, or a long-term tobacco user. Chronic sun exposure, which has long been linked to skin cancer, has also been linked to malignancies of the lips. Genetic factors are also thought to play a role in who gets the condition.
Detecting Oral Cancer
A complete oral cancer screening is included in your routine dental appointment, which is another another incentive to have your teeth evaluated on a regular basis. A visual examination of your lips, tongue, and inside of your mouth, including a look for red or white areas or atypical sores, is part of the screening. Your tongue may be gently moved aside for a better view, and you may be palpated (pressed with fingers) to detect the existence of lumps and swellings. To help check any questionable spots, a special light, dye, or other method may be employed. A biopsy can be conducted quickly if anything looks to be out of the ordinary.
If you notice abnormal sores or color changes in the tissue of your mouth, lips and tongue, they may be a symptom of oral cancer — most, however, are completely benign. But sores or other unusual changes that haven’t gone away by themselves after 2-3 weeks should be examined. Remember, the only way to accurately diagnose oral cancer is through a laboratory report. Early diagnosis, aided by thorough screenings at your regular dental checkups, is one of the best defenses against oral cancer.
 Wisdom Tooth Removal
Wisdom Tooth Removal
The third set of molars, also known as “wisdom teeth,” begin to appear in most people between the ages of 17 and 25. The emergence of these teeth, on the other hand, is frequently fraught with complications. The extraction (removal) of one or more third molars is a rather common treatment, with around 5 million people undergoing the procedure each year. You may be advised to have your wisdom teeth pulled after a comprehensive examination and diagnostic testing such as x-rays or a CT scan. Here are a few common reasons:
- Your jaw may be too small to accommodate all your teeth, leading to excessive crowding and the chance of your wisdom teeth becoming impacted — that is, unable to emerge from the gums, and potentially harmful to adjacent bone or teeth
- Your wisdom teeth may be erupting (coming in) in a crooked orientation, which can damage other teeth or anatomical structures in the jaw, and/or cause bite problems
- If your wisdom tooth does not fully erupt (emerge from the gums), it can increase the chance for bacterial infection
- A cyst (a closed, fluid-filled sac) may develop around the unerupted wisdom tooth, which can cause infection and injury to the adjacent bone or nerve tissue
The excision of wisdom teeth can be a successful treatment for a variety of reasons, including preventing future issues or alleviating a current ailment. However, as with any medical operation, the advantages must be weighed against the minor possibility of complications, and the procedure should be thoroughly discussed.
The Extraction Procedure
Wisdom tooth extraction is normally done in the office by a dentist or an oral surgeon. It’s possible to have the procedure done with just a local anesthetic (numbing shot) to keep you pain-free; but, if numerous teeth are being pulled at once (which is common), a general anesthesia or conscious sedation may be used. Before the procedure, the appropriate type of anesthetic for you will be established.
If the tooth is impacted, the gum tissue at the extraction site may need to be opened after you’ve been properly anesthetized. After that, the tooth will be gently removed. After the extraction, you may need to have the wound sutured (sewn) to help it heal. After the surgery, you will be given some time to recover before returning home. Depending on the type of anesthetic you received, you may require the assistance of another driver.
After the Procedure
The time it takes to recuperate from wisdom tooth extraction is usually only a few days. Rest as much as possible during this time to promote healing, and take any pain medicine as directed. It’s common to have some bleeding at the extraction site; this can be managed by gently biting on gauze pads and changing them as needed, as well as sleeping with the head elevated on pillows rather than flat.
On the first day following the surgery, using an ice pack to the outside of your cheek for a few minutes at a time may help minimize swelling. Starting on day 2, a warm moist heat from a washcloth placed on the cheek may help you feel more at ease. Mouthwashing with warm salt water many times a day might also help ease pain.
For a few days after the extraction, you should eat soft foods and avoid brushing or placing anything in your mouth until your recovery is complete. Because each scenario is unique, be sure to follow the postoperative recommendations given to you; this will ensure that you are as comfortable as possible.
 Have you ever gotten a black eye, a chipped tooth, or a bruised face as a kid? If that’s the case, you may have suffered from facial trauma (hopefully minor!). However, face trauma can be serious in many cases. Auto accidents, sports injuries, work-related incidents, falls, and acts of aggression are all substantial contributors. When you suffer a major facial injury, it’s critical that you receive prompt and comprehensive treatment. That’s why most emergency and trauma facilities have oral and maxillofacial surgeons on call.
Have you ever gotten a black eye, a chipped tooth, or a bruised face as a kid? If that’s the case, you may have suffered from facial trauma (hopefully minor!). However, face trauma can be serious in many cases. Auto accidents, sports injuries, work-related incidents, falls, and acts of aggression are all substantial contributors. When you suffer a major facial injury, it’s critical that you receive prompt and comprehensive treatment. That’s why most emergency and trauma facilities have oral and maxillofacial surgeons on call.
Facial trauma in general involves injuries to the soft- or hard-tissue structures of the face, mouth or jaws — which includes the teeth, jaw and face bones, as well as skin and gum tissue. Treatment of specific specialized locations, such as the area around the eyes, the salivary glands, or the facial nerves, is also possible. Because facial injuries can damage a person’s ability to perform essential living activities (eating, vision, etc.) as well as his or her attractiveness, treatment generally includes a strong emotional component in addition to a physical one. Oral and maxillofacial surgeons, on the other hand, can handle the whole range of facial injuries after finishing a rigorous training program.
Treatments for Facial Injury
Some facial injuries aren’t as serious as others. When a tooth becomes loose or is knocked out, this is a typical occurrence (avulsed). The tooth can often be successfully re-implanted in the jaw if treated quickly. If this isn’t possible, the most effective technique to replace a missing tooth is to use a dental implant.
A fracture of the facial bones, such as the cheekbones, upper or lower jawbones, or eye sockets, is another reasonably common but more catastrophic injury. In theory, it’s treated similarly to a broken arm: the bones are put back in their proper position and immobilized. However, because a cast on the face is not practical, alternative immobilization procedures are required. Wiring the upper and lower jaws together to allow them to recover in the proper alignment is one way; plates and screws can also be used to permanently rejoin the bones.
Because nearly 60% of individuals with severe facial trauma also have major injuries in other parts of their bodies, severe facial trauma is often a life-threatening condition. Oral and maxillofacial surgeons created many of the conventional treatments used in trauma centers throughout the wars in Korea, Vietnam, and the Middle East. Breathing must be restored, blood must be controlled, and neurological damage must be assessed. After that, the reconstructive surgery is completed in one procedure as much as possible.
Preventing Facial Trauma
What is the best way to deal with face trauma? Prevention. Wearing seat belts, wearing adequate helmets and protective gear when playing sports, and avoiding dangerous situations (such as driving while inebriated, sleepy, or preoccupied) can all help keep you safe. Wear a correctly fitted mouthguard if you’re participating in physical activities that pose a risk of facial injury. This small piece of protective equipment can spare you a lot of potential harm.
If you need to go to the emergency room because of a facial injury, make sure to request a consultation with an oral and maxillofacial surgeon so that you get the best care and the best outcome possible.
 Dentistry’s main goal is to protect your natural teeth and keep them as healthy as possible for as long as possible. However, there are situations when having a tooth taken is in your (or your child’s) best interests (removed). For a variety of reasons, this could be the case. Perhaps you have a tooth that has been seriously damaged by trauma or decay, or a wisdom tooth that is impacted and could give you problems in the future. Perhaps your adolescent will need orthodontic treatment soon because he has little space for his adult teeth, a condition known as crowding. Or maybe your younger child still has a baby tooth that refuses to fall out, despite the fact that it’s past its prime.
Dentistry’s main goal is to protect your natural teeth and keep them as healthy as possible for as long as possible. However, there are situations when having a tooth taken is in your (or your child’s) best interests (removed). For a variety of reasons, this could be the case. Perhaps you have a tooth that has been seriously damaged by trauma or decay, or a wisdom tooth that is impacted and could give you problems in the future. Perhaps your adolescent will need orthodontic treatment soon because he has little space for his adult teeth, a condition known as crowding. Or maybe your younger child still has a baby tooth that refuses to fall out, despite the fact that it’s past its prime.
Tooth extraction is usually a pretty regular process, regardless of the reason. The ease with which this minor surgery can be performed depends on the location of the tooth to be extracted in the mouth and the condition of its roots. A front tooth with a single straight root, for example, is easier to extract than a molar with many roots. This is especially true if the molar is an impacted wisdom teeth, which means it is below the gum line and surrounded by bone and gum tissue. Other teeth in its path frequently prevent wisdom teeth from fully erupting (growing in).
Even yet, when done by a skilled hand, tooth extraction is nothing to be afraid of. Keep in mind that, contrary to popular belief, a tooth is not rigidly cemented in its surrounding bone. It is, in reality, connected to the bone by a network of fibers known as the periodontal ligament. These fibers can be easily removed and the tooth liberated by carefully manipulating the tooth.
Reasons for Extracting a Tooth
As previously said, there are a multitude of reasons why a tooth may need to be extracted. Always inquire about the benefits and drawbacks of any dental treatment, including extraction.
- Trauma or Disease — In both of these situations, there are several ways to try and save the tooth. The damaged tooth might need a full-coverage crown, a root canal treatment, or both. But sometimes even these methods are not enough to keep the tooth functioning well and looking good; it might be better to remove the tooth and replace it with a strong and lifelike dental implant.
- Orthodontic Treatment — Teeth are sometimes extracted when there are too many of them for the size of the dental arches (jaws), a situation known as crowding. After an adequate amount of space is opened up through the extraction of one or more teeth, the remaining teeth can be aligned properly. The teeth most frequently removed for orthodontic reasons are the first premolars, which are right next to the eyeteeth (canines).
- Impacted Wisdom Teeth — Early removal of impacted wisdom teeth can prevent damage to neighboring healthy teeth, bone, gum tissue, even nerves and blood vessels. If an impacted wisdom tooth is in a bad position, it’s best to remove it before its roots are fully formed.
- Baby Teeth — If a baby tooth is out of position or not lost in the right sequence, the permanent tooth underneath it might not erupt normally. In this case, removing the baby tooth could prevent a need for orthodontic treatment later on.
The Process of Extracting a Tooth
A radiographic (x-ray) examination is the initial step in any extraction to determine the position of the tooth roots and the condition of the surrounding bone. This will allow for the anticipation of any potential difficulties. To verify that you are healthy enough to undertake the treatment, a comprehensive medical and drug history will be collected, and your anesthetic choices will be addressed.
Local anesthetic is used to numb the teeth to be extracted as well as the surrounding bone and gum tissues. Additional sedatives, such as oral sedatives or conscious sedation administered intravenously, may be employed (into a vein). For more sophisticated (or many) tooth extractions, the latter is frequently required. You won’t even be aware that the procedure was done by the time the anesthesia medication wears off.
Steps are taken to protect the bone that surrounds your tooth while it is being extracted. When a tooth is extracted, a small amount of lab-processed bone-grafting material is sometimes inserted into the socket to assist preserve bone volume. This is especially critical if the extraction will be followed by the implantation of a dental implant, which must bond to existing bone, or orthodontics, which pushes teeth softly through bone.
What to Expect After Tooth Extraction
The socket will be covered with sterile gauze and light pressure provided for 10-20 minutes to control any bleeding after your tooth is pulled. This could also be done with little sutures (stitches). Some mild to moderate post-operative discomfort and/or edema is normal. The majority of symptoms can be controlled by taking non-steroidal anti-inflammatory medicines like ibuprofen and/or aspirin on the day of surgery. Antibiotics may also be recommended to guarantee infection-free recovery. It may also be beneficial to apply ice packs to the outside of your jaw and consume softer meals until you feel more at ease. Everything should be normal again in a few days.
 There’s so much dentistry can do these days to make your mouth healthier and your smile more beautiful. Yet many people don’t take advantage of this because of a long-standing fear of dental treatment. If you are one of these people, rest assured that it’s possible to have an experience that’s free of anxiety and pain. This can be accomplished by blocking your sensations of pain with local anesthetics or by giving you medication that can help you relax. Sometimes both are needed to ensure maximum comfort, especially if you are someone for whom the injections that deliver local anesthetics are themselves a major source of anxiety.
There’s so much dentistry can do these days to make your mouth healthier and your smile more beautiful. Yet many people don’t take advantage of this because of a long-standing fear of dental treatment. If you are one of these people, rest assured that it’s possible to have an experience that’s free of anxiety and pain. This can be accomplished by blocking your sensations of pain with local anesthetics or by giving you medication that can help you relax. Sometimes both are needed to ensure maximum comfort, especially if you are someone for whom the injections that deliver local anesthetics are themselves a major source of anxiety.
When you are afraid of dental treatment, your guard goes up and your pain threshold goes down; anticipating that something will hurt makes you hypersensitive to every sensation — even sound. If this describes your experience in the dental chair, then you might benefit from sedatives that can be given during your visit to make that anxiety melt away.
Before any particular sedative is recommended, you will be asked to provide your complete health history, including any medications you are currently taking — both prescription and over-the-counter. It is also important to know if you smoke or drink. On the day of your treatment, you may need to have someone drive you to and from your appointment as certain medications take time to wear off.
Ways to Relieve Anxiety
Oral Sedation — Oral sedation (given by mouth) is a popular option for many people precisely because it does not require the use of needles. Oral sedatives are either swallowed whole in pill form or can be dissolved under the tongue. Both methods work in a matter of minutes. A variety of oral sedative and anxiolytic (anxiety-dissolving) medications have been developed through extensive research and testing to make your experience of dental treatment as comfortable and relaxing as possible. All have long safety records after decades of use, and several even have “amnesic” properties, meaning you will remember little to nothing, even though you are conscious throughout the treatment. Commonly prescribed medications include Valium®, Halcion®, Sonata®, Ativan®, Vistaril®, and Versed®.
Inhalation Conscious Sedation — Nitrous oxide, a sedative you inhale, has been used in dental offices for nearly 100 years. It is a relatively poor pain reliever but a very good anti-anxiety medication. It is administered through a nasal hood, which resembles a small cup that is placed over your nose. The oxygen mixed with nitrous oxide provides a light-headed or even euphoric feeling, which is quick to wear off so there is no “hangover” effect. All bodily functions remain essentially normal during the use of this sedative, which is very safe.
IV Conscious Sedation — Sedatives delivered directly into the bloodstream intravenously (into the vein) are more potent than when taken orally, and the amnesic effects may be more profound. Because IV sedation has an almost immediate effect on the body and its functions — including heart rate, blood pressure and breathing — there is a higher degree of risk associated with it than with other types of sedatives. There is also a higher level of training required for those who administer it. As with all sedation (except nitrous oxide), you must be monitored with specialized equipment throughout your IV sedation treatment. The main advantage is that drugs administered this way work immediately and the level of sedation can be adjusted more quickly and easily. And with most sedatives, you won’t remember a thing about your dental procedure after the sedative wears off.
 Do you think of bone as a stiff, unyielding substance that never changes? Bone, in fact, is constantly remodeled by your body, with new bone cells being added and old ones being removed. This procedure can be beneficial or damaging to the bone that supports your teeth. The elasticity of the jawbone, for example, allows an orthodontist to use braces to reposition teeth into a better position. However, if a tooth is lost as an adult, the resulting bone alterations can have catastrophic repercussions.
Do you think of bone as a stiff, unyielding substance that never changes? Bone, in fact, is constantly remodeled by your body, with new bone cells being added and old ones being removed. This procedure can be beneficial or damaging to the bone that supports your teeth. The elasticity of the jawbone, for example, allows an orthodontist to use braces to reposition teeth into a better position. However, if a tooth is lost as an adult, the resulting bone alterations can have catastrophic repercussions.
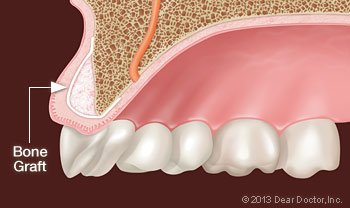
When teeth are removed, the bone that once surrounded them begins to resorb (melt away). When you have periodontal (gum) disease, you can lose tooth-supporting bone as well. Your facial features will sag if you lose enough teeth and bone, giving you an older appearance; it can also make therapy to restore lost teeth more difficult. Fortunately, contemporary bone grafting techniques allow for the reconstruction of missing bone. By strengthening your jawbone, allowing for more successful tooth replacement, and providing support for your facial features, this can help both your health and looks.
Bone grafting is a small surgical operation usually performed in a dentist’s office. An incision in your gum is made to give access to the bone underlying it, and grafting material is subsequently applied. The grafting material is usually processed bone minerals, which your body will deposit new bone cells around.
The grafting material can come from your own body, but it is frequently bone from an animal or human donor that has been sterilized and made safe in a laboratory. It could possibly be a man-made substance. Grafting material is available in a variety of forms, including powder, granules, putty, and a gel that can be injected via syringe. The graft will operate as a scaffold for your body to grow new bone, and it will be covered by a collagen membrane for maximum bone regeneration.
Uses for Bone Grafts
Bone grafts are used in dentistry to accomplish the following treatment goals:
- Saving Teeth — When severe periodontal disease causes bone loss, teeth can become loose and at risk of being lost. In order to save them, the bone around them can be regenerated through grafting; this increases bone support and helps keep them in place.
- Tooth Extractions — These days, it is very common to deposit bone grafting material into a tooth socket after a tooth has been removed. That way, should you want to replace your tooth with a dental implant later on, that option will be available.
- Dental Implants — A titanium post placed in the jawbone is linked to a highly realistic dental crown in this ideal tooth-replacement device, permanently replacing the missing tooth. To achieve their great performance and high success rates, implants require sufficient bone volume and density. If you’ve previously had bone loss, a graft can help you regrow enough bone to successfully place the implant.
What to Expect from Bone Grafting
The technique for inserting a bone graft normally only requires local anaesthetic, though oral or IV (intravenous) sedatives might be used to induce a more relaxed state. You may experience some soreness in the area following the surgery because a small incision is created in your gum tissue to allow access to the bone that will receive the graft. Over-the-counter anti-inflammatory medications and/or pain killers, as well as ice therapy after the procedure, can frequently help. Any discomfort should last no more than a day or two. Your body will then replace the transplant with its own bone over the next several months, reversing the bone loss you’ve experienced.
 You might think that when you go to the dentist for an examination, the attention will be on your teeth. That’s often true, but don’t forget that a variety of other aspects of the oral and face anatomy are also inspected. These include both within and outside the mouth (such as the lips, gums, hard and soft palate, and tongue), as well as places around and inside the mouth (such as the lips, gums, hard and soft palate, and the tongue) (the skin, muscles and glands in the neck, and the temporomandibular joint). In fact, a thorough dental exam may be your first line of defense when it comes to diagnosing some oral or systemic (whole-body) disorders.
You might think that when you go to the dentist for an examination, the attention will be on your teeth. That’s often true, but don’t forget that a variety of other aspects of the oral and face anatomy are also inspected. These include both within and outside the mouth (such as the lips, gums, hard and soft palate, and tongue), as well as places around and inside the mouth (such as the lips, gums, hard and soft palate, and the tongue) (the skin, muscles and glands in the neck, and the temporomandibular joint). In fact, a thorough dental exam may be your first line of defense when it comes to diagnosing some oral or systemic (whole-body) disorders.
What methods are used to detect disorders in the mouth? Most of the time, it’s straightforward: You’ll be asked if you’ve seen any changes or if you’re suffering any symptoms. Your face, mouth, and neck will be visually examined, and some areas of your body may be palpated (gently felt with fingers) or probed (touched with a small instrument). Additional tests or diagnostic imaging (X-rays or other methods) may be utilized to help with the diagnosis if necessary.
An anomaly, such as a lesion (an uncommon localized alteration in your tissues), is occasionally discovered and requires additional investigation. Lesions might look like white or red spots or lumps (tumors), however they are usually harmless. However, it is often preferable to err on the side of caution and conduct a biopsy to be certain. It may be necessary to make a small incision and remove a portion of the questionable area. The tissue sample will be submitted to a pathologist, who will look for symptoms of disease under a microscope.
Some Oral Diseases To Look For
Oral cancer is the most important condition to search for during an exam, both because it can be life-threatening and because early discovery has been shown to improve survival rates. It’s crucial to note, however, that the vast majority of odd growths are benign. Other oral disorders that could be detected include:
- Fibroma, a thickened mass that may feel like a lump in the lining of the mouth.
- Leukoplakia, a condition that causes white patches to form inside the mouth. While usually benign, the lesions may be precancerous and are often biopsied.
- Lichen Planus, an inflammatory disease that sometimes causes discomfort.
- Mucous Membrane Pemphigoid, an autoimmune disease that may cause oral lesions, but is not life threatening.
- “Pregnancy Tumors,” benign red swellings that may form on gum tissue of pregnant women due to hormonal changes.
Additionally, several systemic disorders (such as diabetes, Crohn’s disease, and heart disease) can cause symptoms in the mouth. We’re always on the watch for warning symptoms of these potentially fatal illnesses.
When a Biopsy Is Needed
Although the majority of oral lesions are benign, a biopsy will almost certainly be conducted if there is any chance that the growth is cancerous or pre-cancerous. This could be a simple in-office treatment or a hospital procedure, depending on how much tissue needs to be removed. The surgery usually only requires local anesthetic and takes only a few minutes. Incisions are frequently closed with self-dissolving sutures that do not require removal.
Because the oral tissues are densely packed with blood vessels, some bleeding is to be expected for a while following. Follow-up instructions, such as how to control swelling and discomfort, when to take medicine, and what to eat and drink, will be given as needed. Resting and maintaining proper dental hygiene will also assist you in returning to normal as early as possible. You will be sent the results once the pathology report is completed (typically in a few days).
Using today’s modern dental and orthodontic treatment technologies, abnormalities with the bite or tooth alignment can be rectified in many cases. Skeletal and dental anomalies, on the other hand, aren’t always straightforward to correct, even with the most advanced non-surgical procedures. Corrective jaw surgery (also known as orthognathic surgery) may be recommended at this point.
While jaw surgery may appear to be a difficult and time-consuming procedure, it is not necessarily so. It’s frequently done as a normal in-office operation, such as to remove impacted wisdom teeth or install dental implants in the jaw. It can, however, be used to treat serious orthodontic issues concerning the interaction between the teeth and jaws, such as underbites and congenital anomalies related to jaw development. It may even aid in the treatment of sleep apnea, a potentially fatal disorder.
Who Can Benefit From Jaw Surgery
Orthognathic (jaw) surgery may be beneficial for those who have abnormalities with their jaws, teeth alignment, or facial asymmetries that make chewing, talking, sleeping, or carrying out daily tasks difficult. These treatments can also be utilized to correct aesthetic concerns including a projecting jaw, a congenital deformity, or a facial appearance that is imbalanced.
It can be established if you are a candidate for orthognathic surgery after a thorough examination. In general, you’ll start with orthodontic therapy if it can solve the problem. While orthodontics can successfully align the teeth, the jaws must occasionally be brought into alignment as well. Most orthodontic products, such as braces and retainers, will be used both before and after the surgical phase of treatment to guarantee a successful — and aesthetically acceptable — outcome.
The following are some of the conditions that can be successfully treated with corrective orthognathic surgery:
- Open bite, protruding jaw or receding chin
- Congenital defects such as a cleft palate
- Malocclusions (bite problems) resulting from underbites or severe overbites
- Obstructive Sleep Apnea, when more conservative methods fail
- Difficulty swallowing, chewing, or biting food
- Chronic jaw or jaw joint (TMJ) pain and headache
- Unbalanced facial appearance from the front or side
- Inability to make the lips meet without straining
- Chronic mouth breathing and dry mouth
- Facial trauma
The Surgical Procedure
While each patient’s needs are unique, there are some common elements in the procedure that can be outlined. Consultation and planning among members of the dental team, including the restorative or general dentist, orthodontist, and oral surgeon, is the initial (and perhaps most crucial) component. Orthodontic treatments and surgical procedures may be part of your overall strategy. A step-by-step strategy for the entire procedure will be produced using diagnostic photos, 3-D models, and advanced software. In many circumstances, your doctor will be able to show you a picture of how you’ll look once your treatment is completed.
The operation may take place in a hospital or in an office environment, with the sort of anesthesia that is best for the procedure and your comfort. Because the operation is usually done inside the mouth, there are rarely any visible scars. Minor pain and swelling can be managed with over-the-counter or prescription pain relievers after the surgery. Following the surgery, a soft or liquid diet may be prescribed for a period of time.
Your condition, as well as your progress through each phase of the treatment plan, will be thoroughly evaluated following surgery. When it’s finished, you’ll be able to take advantage of increased functionality and a more appealing appearance.
Meet Your Award-Winning Dentists in Mission Viejo & Fullerton, CA








Our Dental Services
General Dentistry
Dental Implants
Emergency Care
Pediatric Dentistry
Oral Surgery
Orthodontics
The Proof is in our Patients

2 Convenient Locations
Our Fullerton, CA Office
1950 Sunny Crest Dr., Ste #1100
Fullerton, CA 92835
Working Hours
Our Mission Viejo, CA Office
24896 Chrisanta Drive, Suite #110
Mission Viejo, CA 92691







