Endodontics & Root Therapy in Southern California
OC Smile, Protecting and Treating Roots and Dental Pulp
Root Canal Therapy in Mission Viejo
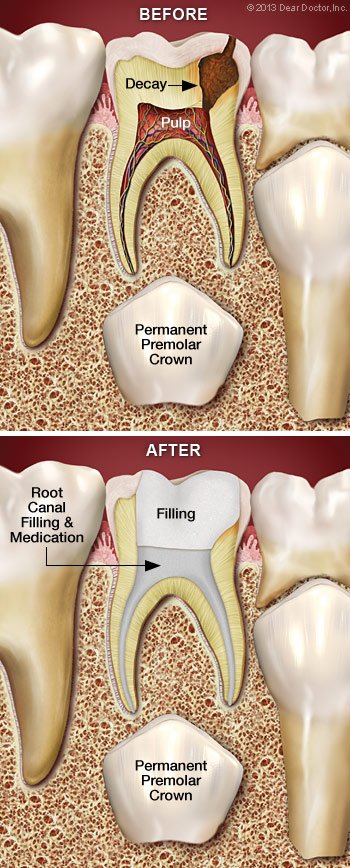
When a tooth’s pulp becomes infected or inflamed, which can happen as a result of severe dental decay, a crack in the tooth, or some other type of trauma to the tooth, root canal therapy is required. Severe throbbing pain in the tooth or more widespread discomfort in the head and neck are signs of infection. Infections can harm the jaw and spread to other teeth if they are not treated right.
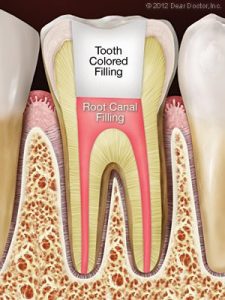
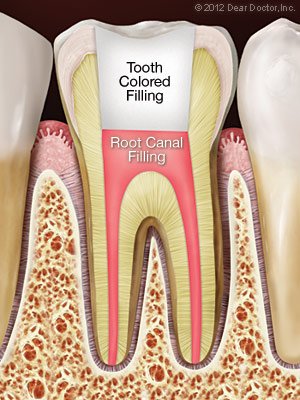
Root canals are outpatient procedures carried out under local anaesthetic in the offices of OC Smile Dental & Orthodontics. The decomposing pulp will be carefully removed, the region will be cleaned, and a special putty will be used to cover the cavity. In order to seal and protect the tooth, we frequently finish the treatment by placing a crown on it.

Microsurgery in Fullerton
When doing root canals, dental implants, and other operations, OC Smile Dental & Orthodontics makes use of contemporary microsurgery equipment that enables us to see great detail and work with precision. Microsurgery in medicine is essentially any type of surgery that needs a microscope, and dental operating microscopes of today are a significant improvement over previous technology. We can enlarge surgical areas up to 20 times the conventional views using fiber optic lighting. Dental operating microscopes are more adaptable and simpler for us to use than more conventional magnification tools, which can only magnify objects up to six times the size they normally do.
With the use of this technology, we can perform incisions on our patients with greater accuracy and restraint. Less bleeding, inflammation, and pain result from this. Treatment is completed more quickly, and the results are better. For the comfort of our patients, we welcome modern technologies at OC Smile.
The “Root” of the Problem
What could contaminate the pulp tissue and result in root canal issues? Untreated dental decay is one risk factor for infection since it might open the door for bacteria from the tooth’s surface to penetrate deeply. The pulp of a tooth may get infected by germs through a crack or fracture.
Tooth or pulp may also be harmed by dental trauma, such as that caused by a sports injury, or it may be made vulnerable to infection. Many fillings or restorations on the same tooth or other extensive dental procedures might be problematic. Occasionally, even basic dental procedures like orthodontics can eventually result in root canal issues.
Endodontic Treatment in Mission Viejo & Fullerton, CA
Although the classic joke “I’d rather have a root canal” still makes people chuckle, root canal issues are no laughing matter. It’s crucial to keep in mind that root canal therapy helps pain, not causes it. A conventional root canal is performed with local anesthetics, and the discomfort is comparable to getting a filling. Here is what to anticipate:
The first step will be to undergo anesthesia, which is typically a numbing shot. For many people, this marks the end of the worst. The pulp chamber and root canals are then accessible through a small hole that is created in the tooth’s surface. Then, tiny tools are used to remove dead and dying tissue from inside the constrained channels, frequently with the help of a microscope. Then a safe, inert substance is used to plug these channels after they have been cleaned and sterilized. The tooth’s hole is finally shut to stop contamination.
With the purpose of eliminating infection-causing factors and averting further issues, more endodontic procedures could be suggested. It might be required to have a restoration (such as a crown) put on the tooth after an endodontic operation in order to return it to full functionality and cosmetic appeal. The restored tooth should then last for many years with good care.
Root Therapy in Fullerton, CA – Best Root Canal Dentist Near Me - Endodontic Dentists Proudly Serving Mission Viejo & The Surrounding Areas
 Root canal therapy, commonly known as endodontics (“endo” means within, “dont” means tooth), is a group of specialist operations used to treat issues with the delicate pulp (nerve) tissue inside the tooth. While some people wrongly believe it is a particularly painful process, it is usually no more painful than having a filling. It’s actually one of the most efficient treatments for certain types of tooth pain.
Root canal therapy, commonly known as endodontics (“endo” means within, “dont” means tooth), is a group of specialist operations used to treat issues with the delicate pulp (nerve) tissue inside the tooth. While some people wrongly believe it is a particularly painful process, it is usually no more painful than having a filling. It’s actually one of the most efficient treatments for certain types of tooth pain.
When infection or inflammation develops in the pulp tissue of the tooth, a root canal operation is required. Pulp tissue is made up of blood vessels, connective tissue, and nerve cells, which is why a malfunction here can cause severe discomfort. The discomfort may fade away over time… at least briefly. The infection, on the other hand, will not go away without therapy. It can result in a dental abscess and possibly cause systemic issues in other sections of the body.
Root Canal Treatment Is Your Friend
“I’d rather have a root canal…” is a joke we’ve all heard. This remark about the operation being likened to something truly dreadful may be amusing, but putting off necessary endodontic treatment is no laughing matter. The notion that a root canal operation will always result in complications and pain is an old wives’ tale. It’s true that infection or inflammation in the pulp of the tooth can cause agonizing pain. However, you should keep in mind that a root canal just relieves the acute pain; it is not the cause of the discomfort.
Do you need another reason to get a root canal? Consider this: When a natural tooth is saved by root canal treatment and restoration, you can avoid the issues that often emerge when teeth must be extracted. These include tooth migration or shifting, which can cause chewing problems; the necessity for bridgework or dental implants, which can be expensive and time-consuming; and even the ultimate loss of bone structure in the location of the missing tooth.
Causes of Root Canal Problems
Infection and inflammation of the pulp tissue of the tooth cause root canal complications. Deep dental decay is one possible source of infection. Bacteria will gradually work their way down to the core of the tooth, where they may infect the pulp tissue if left untreated. Bacteria may also get into touch with the pulp through broken or damaged teeth. Bacteria can gain access to the tooth’s pulp through any crack in the protective enamel coating.
Trauma to the tooth, such as those that are caused by a sports injury or an automobile accident, is another common cause of pulp tissue destruction. In this instance, it’s critical to seek treatment right away, both to save the tooth and to avoid future complications.
In some circumstances, significant dental work might damage the pulp tissue, necessitating a root canal. This form of injury is more likely if you have many fillings or restorations on the same tooth. Root canal complications might occur as a result of common operations such dental crown preparation or orthodontics.
What to Expect During Root Canal Therapy
Don’t panic if a checkup reveals that you require root canal therapy; it’s one of the most common and effective operations in the dental armory, and it may often be completed in just one visit.
The root canal procedure usually begins in the same way that a filling does, with no more pain: an anesthetic is used to numb the tooth and surrounding area. For a lot of patients, the worst is already behind them.
The pulp chamber and root canals are then accessed through a small incision in the damaged tooth’s surface. To remove the dead and dying pulp tissue from inside these narrow pathways, tiny devices are employed, sometimes with the help of a microscope. The chamber and empty canals are then cleansed, disinfected, and readied for the inert, biocompatible substance to be filled. Finally, sticky cement is utilized to close the tooth’s opening, preventing infection in the future.
Following root canal treatment, your tooth may feel some sensitivity or tenderness for a few days. Ibuprofen and other over-the-counter pain medicines are usually beneficial, although prescription medications may be prescribed if necessary. It may be beneficial to avoid biting hard on the impacted tooth during this time. All of these symptoms, on the other hand, should only last a short time.
A crown or other treatment is frequently required to further safeguard the tooth and restore it to full functionality. Restorations come in a variety of shapes and sizes, ranging from standard gold crowns to high-tech dental replicas made of tooth-colored material. In any case, you’ll have made a long-term investment in maintaining your dental health.
Signs and Symptoms of Root Canal Problems
How can you tell whether you require a root canal? It’s sometimes painfully evident. If you are experiencing frequent and severe pain and pressure in your mouth, as well as visible swelling and high sensitivity in your gums, it is apparent that you require immediate evaluation and treatment. Sharp pain when biting down on food is another unmistakable sign of pulp tissue injury. Pain that persists after eating hot or cold foods is also a sign of trouble. If you observe any of these symptoms, you should seek medical attention right once.
 Root canal therapy is usually successful in permanently alleviating tooth discomfort and preventing infection of the soft tissues deep within the teeth and gums. However, like with any medical surgery, the body may not always mend as we want. You may experience pain in the damaged tooth again after a period of time, or x-rays may suggest that infection is still present near the tooth’s roots even if you have no symptoms. In that situation, root canal retreatment may be required.
Root canal therapy is usually successful in permanently alleviating tooth discomfort and preventing infection of the soft tissues deep within the teeth and gums. However, like with any medical surgery, the body may not always mend as we want. You may experience pain in the damaged tooth again after a period of time, or x-rays may suggest that infection is still present near the tooth’s roots even if you have no symptoms. In that situation, root canal retreatment may be required.
There are a number of reasons why your root canal treatment did not work out the first time. The “canals” are slender, forking channels deep inside the tooth that encase nerves and blood vessels: the soft “pulp” of the tooth. Some may have gone undetected or failed to respond to treatment the first time because they are so small and complicated. A delayed or inefficient crown restoration, new dental decay, progressive gum disease, or a cracked or fractured tooth are all possibilities for recontamination of the canals. Reinfection could occur under any of these circumstances.
If your root canal (endodontic) treatment has failed, the first step is to weigh your options. Endodontic surgery or tooth extraction (removal) may be options in addition to retreatment. A missing tooth, on the other hand, should be replaced as soon as possible with a dental implant, a bridge, or a partial denture – none of which are straightforward or inexpensive solutions. That’s why, wherever feasible, we prefer to assist you in keeping your natural teeth.
The Retreatment Procedure
If endodontic retreatment is right for you, it’s identical to a regular root canal with a few extra precautions. Any existing restorations on your tooth — crowns, for example — will be adjusted to provide access to the root canal filling material after you’ve been anesthetized (typically with a numbing shot). Making a small aperture into the inner part of the tooth, removing filling material or blockages, and cleaning the pulp chambers with microscopic instruments is usually how this is done.
Additional canals or strange structures are carefully searched for using a microscope and light. It’s possible that the therapy will be completed in a subsequent session if the treatment becomes highly difficult. After all of the canals have been cleaned and disinfected, they will be filled and sealed with inert material. After that, the tooth will receive a temporary filling. At some point in the future, a permanent restoration will be needed.
Is Root Canal Retreatment My Best Option?
Medicine and dentistry are both an art and a science, and neither can promise that any surgery will be successful 100 percent of the time. While endodontic retreatment is more difficult than initial root canal therapy, it has a high success rate in many cases. Furthermore, because the field of endodontics is always changing, it may be possible to apply new treatments that weren’t available when your first root canal was performed.
Dentists take their obligation to educate you understand the dangers, benefits, and alternatives to root canal treatment very seriously. When we propose retreatment, it’s because we believe it’s the greatest approach to protect your natural teeth and ensure that you may enjoy them for many years to come.
 In some cases, root canal treatment fails to resolve an infection in the tissues around a tooth’s roots. An apicoectomy, a small surgical operation, may be recommended at that point. This operation is classified as endodontic microsurgery since it is frequently performed with the help of a microscope and other small specialized equipment. An apicoectomy is the most common type of root canal surgery, and it entails removing a tiny section of the apex (tip) of the tooth’s root, as well as any infected surrounding hard or soft tissue.
In some cases, root canal treatment fails to resolve an infection in the tissues around a tooth’s roots. An apicoectomy, a small surgical operation, may be recommended at that point. This operation is classified as endodontic microsurgery since it is frequently performed with the help of a microscope and other small specialized equipment. An apicoectomy is the most common type of root canal surgery, and it entails removing a tiny section of the apex (tip) of the tooth’s root, as well as any infected surrounding hard or soft tissue.
What circumstances would necessitate an apicoectomy? There could be a number of causes for this, including a blocked or inaccessible canal, an anatomical irregularity, or a fracture or crack in the root of the tooth. The operation is usually indicated only after one or more root canal treatments have failed. The treatment is frequently a good way to treat a persistent infection because this type of disease develops around the apex of the root.
Diagnostic photographs (such as X-rays) of the damaged tooth and surrounding bone, as well as a thorough evaluation of your medical history, including drugs you take (both prescription and non-prescription), and other considerations are reviewed before an apicoectomy treatment. The reasons for an apicoectomy will be presented to you if one is recommended.
The Apicoectomy Procedure
You won’t feel any discomfort because root canal surgery is usually done under local anaesthetic, such as a numbing shot. A small incision in the gum is made to reveal the infection near the end of the tooth’s roots, which begins the treatment. The diseased tissue, as well as a few millimeters of the root tip itself, is then removed. A dye may be used to help see cracks or fractures; if the tooth is damaged, it may be best to extract (remove) it now rather than waiting until the apicoectomy is finished.
The microscopic canals are then examined using a microscope and light. They’ll be cleaned with an ultrasonic device before being filled with an inert substance and sealed with a tiny filler. A little bone graft may be put at the damaged spot to complete the treatment, and the gum tissue surrounding the tooth’s root will be sutured (stitched) up. As the surgery nears completion, X-rays may be taken. After that, you’ll be given postoperative instructions and sent home. The majority of apicoectomies take between 30 and 90 minutes to complete.
You may notice some swelling and pain in the treated area after the operation. To relieve pain, over-the-counter non-steroidal anti-inflammatory drugs (such as ibuprofen) are usually sufficient. You should be able to resume normal activities the next day, although for a few days afterward, you should avoid eating hard or crunchy foods or violently brushing your teeth. If your sutures don’t dissolve on their own, you’ll be asked to come back in a week to have them removed.
The Goal: Saving Your Tooth
Although apicoectomy is usually a safe and effective technique, every sort of minor surgery has some risk. As a result, apicoectomies are only suggested if other root canal treatments have failed. In most circumstances, extraction of the tooth is an alternative option. Our goal as dentists, on the other hand, is to help you keep your natural teeth for as long as feasible.
While there are good tooth replacement options (such as dental implants), they need additional, more sophisticated procedures and can be pricey. An apicoectomy is a permanent and cost-effective procedure that can help your tooth last the rest of your life.
 Your teeth are remarkably durable, rooted in your jaw and covered by an exterior coating of resistant enamel, yet they can still chip, crack, or even break. Indeed, there is evidence that our teeth are cracking at an unprecedented pace now. This could be because people are living longer, giving teeth more time to deteriorate, or because our stress levels are rising (which may cause teeth clenching and grinding).
Your teeth are remarkably durable, rooted in your jaw and covered by an exterior coating of resistant enamel, yet they can still chip, crack, or even break. Indeed, there is evidence that our teeth are cracking at an unprecedented pace now. This could be because people are living longer, giving teeth more time to deteriorate, or because our stress levels are rising (which may cause teeth clenching and grinding).
Tooth fractures can also be caused by biting on hard objects, an injury to the mouth or by big cavities that undermine the tooth’s structure. However, regardless of the origin, there are a number of signs that suggest a broken tooth, as well as a variety of treatments we can provide, depending on the severity of the injury.
Small chips on the edges or cusps of teeth that cause no symptoms can be treated with cosmetic bonding or other techniques. Deeply fractured teeth, on the other hand, can be a severe problem. The sooner they are treated, the more likely the impacted tooth will be saved. Let’s take a closer look at the different types of fractures teeth can get, as well as the symptoms they can cause.
Minor Cracks (craze lines)
Most of the time, these microscopic fissures in the outer enamel of the tooth create no symptoms and don’t require treatment. However, if you have tooth pain, these fissures should be checked and maybe corrected. That’s because it’s impossible to tell if these fissures are limited to the enamel or extend into the dentin (inner core) of the tooth without a thorough inspection. While the tiniest craze lines aren’t visible on X-rays, they may typically be spotted by feeling (with a little device called an explorer), using a “bite stick,” or with special dye stains or high-magnification instruments.
Vertical Cracks
This sort of crack usually begins on the chewing surface and progresses to the roots, but it can also start in the root and progress to the crown. In either case, the tooth is not totally divided into two pieces. Depending on the severity of the fracture, you may only experience minor discomfort in response to temperature changes (such as when drinking hot or cold beverages), or you may have acute pain when chewing. In any case, you shouldn’t ignore the signs and symptoms since broken teeth require immediate dental care to prevent them from worsening. Tooth extraction may be required if the cracks continue to spread.
Deep Fractures or Split Teeth
When a tooth is seriously fractured, the distinct portions of the tooth might be separated from one another, and the pulp is frequently irritated and painful. This condition necessitates rapid treatment, and saving the damaged tooth is rare.
Treatment for Cracked Teeth
The optimal treatment for a cracked tooth is determined by the degree and severity of the injury. It’s often easy to seal a minor crack with restorative materials if it’s discovered early enough. Root canal therapy is usually required for larger breaks that involve the pulp of the tooth. After that, the tooth’s visible structure can be reconstructed with a crown or “cap.” Additional operations may be suggested in some cases in order to save the tooth. However, in the most extreme circumstances, the tooth will have to be extracted.
The best way to deal with broken teeth is to avoid them in the first place! When playing sports, wearing adequate protective equipment (such as a custom-fitted mouthguard) and remaining aware to harmful situations (such as distracted or impaired driving) can help you stay safe. Regular dental exams, in which your teeth are carefully examined for early signs of a disease, can also help. If you have any symptoms that could indicate a cracked tooth, don’t wait to see a dentist: the sooner it’s treated, the more likely it is to be saved.
Root canal therapy is a safe and efficient approach to relieve dental pain and prevent the loss of a tooth due to disease or injury. However, if a root canal is recommended for your young child, you may wonder why: after all, won’t that baby tooth fall out in a few years?
True, between the ages of 6 and 12, the primary (baby) teeth are normally gone. However, there are some compelling reasons to try to save baby teeth with root canal treatment for as long as feasible rather than removal those that have been damaged by trauma or infection.
For starters, primary teeth perform the same duties as adult teeth, and a lost tooth at any age might create speaking and eating difficulties. Another significant function of baby teeth is that they act as cues for the optimal placement of permanent teeth. Permanent teeth tend to develop crookedly without primary teeth to assist them in, becoming slanted or crowded as a result of insufficient space. This can lead to bite issues that will likely require substantial orthodontic treatment in the future.
Saving The Tooth Is Always Best
The soft pulp inside the tooth, in contrast to its hard exterior surface, is densely packed with blood vessels and nerves. Tooth sensitivity and pain are common indicators of problems in this area. Radiographs (x-rays) are frequently required when these symptoms appear to determine that the pulp is sick or dying. Treatment is required at this point, before an abscess or additional infection develops.
In severe circumstances, the tooth may need to be extracted and replaced with a space maintainer to close the gap. However, space maintainers frequently fail to entirely restore the tooth’s functionality. Furthermore, they are prone to become loose and must be continually maintained. Other therapeutic options are preferred if at all possible, such as:
- Indirect pulp treatment. If pulp damage is minimal, it’s possible to remove most of the decay (but not the pulp), apply an antibiotic, and then seal the tooth up again; that’s referred to as an “indirect” treatment.
- Pulpotomy. Alternatively, if decay is limited to the upper portion of the pulp, we may recommend a “pulpotomy.” This involves removing the damaged part of the pulp, stabilizing the remaining healthy portion, and then disinfecting and sealing the tooth. This “partial” root canal is a time-tested technique that’s successful in many cases.
- Pulpectomy. If pulp tissue is infected through the entire tooth structure, a pulpectomy may be needed, which requires the removal of all pulp tissue. The canals are then disinfected, shaped, then filled and sealed with inert material. Afterwards, the crown (visible part) of the tooth will be restored. This resembles traditional root canal therapy, with a crucial difference: The sealant we use in children is capable of being dissolved by the body. That way, when it’s time for a permanent tooth to erupt, the baby tooth’s roots can be naturally absorbed and tooth development can proceed normally.
Preparing for Your Child’s Root Canal Treatment
As you undoubtedly already know, most of the root canal myths you’ve heard are just untrue. In fact, the procedure is usually painless, but it is very effective at relieving tooth pain! Dentists are skilled in numbing the pain sensation with anaesthetic and are skilled at calming children’s worries. While it’s reasonable that you’re worried, it’ll help if you don’t let your child sense your fear. A soothing voice and a gentle touch can go a long way toward reducing stress.
Following a comprehensive assessment, the best treatment options for your child will be suggested. These procedures are standard, and you will be given information on how to proceed. A root canal is nothing to be afraid of: think of it as a procedure that could save your child from tooth pain in the short term and a lot of corrective dental work in the long run.
 If you’ve been told you need root canal treatment, you might feel a little concerned. Not to worry – root canal therapy is a common procedure in dentistry that can ease tooth discomfort and extend the life of your teeth. You’ll see why this surgery is necessary as you learn more about it – and how it will leave you in significantly better shape than you were before. Here are some frequently asked questions and their answers.
If you’ve been told you need root canal treatment, you might feel a little concerned. Not to worry – root canal therapy is a common procedure in dentistry that can ease tooth discomfort and extend the life of your teeth. You’ll see why this surgery is necessary as you learn more about it – and how it will leave you in significantly better shape than you were before. Here are some frequently asked questions and their answers.
What is a root canal?
The tiny, narrow channels that branch from a central, hollow space in your tooth down to the ends of the tooth roots are referred to as “root canals” by dentists. The word can also be used to refer to “root canal treatment,” which is a process that saves a tooth when the soft tissue deep inside it becomes irritated or diseased.
Why do I need root canal treatment?
If the pulp of a tooth becomes inflamed or infected as a result of decay or injury, the tissue must be removed to save the tooth and prevent the infection from spreading. You don’t require the pulp as an adult; its principal function is to help tooth formation in children.
Is there an alternative?
You could have the tooth taken completely, but it’s usually preferable to try to save it, especially since root canal therapy is common and has a high success rate (over 90 percent ). Other difficulties, such as bite problems from teeth shifting position, difficulty swallowing, and loss of jawbone volume and density, can be avoided if the tooth is saved.
Is root canal treatment painful?
In most cases, the treatment is no more painful than a filling. Root canal therapy has a terrible reputation, but it is unwarranted; in this case, the disease, not the remedy, is to blame. In other words, the infections that necessitate treatment are often unpleasant because they inflame tissue that is densely packed with nerves and thus extremely sensitive. This pain is actually relieved with root canal therapy!
What will happen during the procedure?
After numbing the area, the pulp chamber and canals are accessed through a tiny hole in the crown (top) of your tooth. The diseased tissue is removed, and the pulp chamber and canal(s) are disinfected from the root end to the pulp chamber (s). Front teeth have one root and, in most cases, one canal; rear teeth have two or three roots and, in most cases, three or four canals. Those canals, as well as the pulp chamber, are filled with a biocompatible inert material and sealed with adhesive cement. A temporary filling will be applied to the access hole.
What will happen afterwards?
For a few days, your tooth may be sensitive, but any pain may usually be eased with over-the-counter pain relievers or anti-inflammatories like ibuprofen. You’ll be told not to chew on that tooth until it gets a permanent filling, which should happen within a few days. A full-coverage crown may be required depending on how badly the tooth was injured to begin with. We’ll talk about those alternatives with you.
How can I avoid the need for root canal treatment in the future?
Brush and floss your teeth every day to keep them free of decay. Avoid acidic beverages like soda and eat a balanced, low-sugar diet. Have expert cleanings and exams on a regular basis. If you participate in sports, a custom-made mouthguard can help protect your teeth from injury.
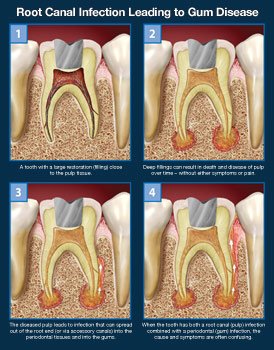 When you have discomfort in your mouth, it’s not always easy to figure out which tooth is to blame. Other times, the discomfort is more broad, generic, or difficult to pin down. It can be difficult to pinpoint exactly what problem or mix of disorders is producing the symptoms you’re experiencing at times. When an infection exists in the root canals of a tooth as well as the gum tissue surrounding it, this may be the situation.
When you have discomfort in your mouth, it’s not always easy to figure out which tooth is to blame. Other times, the discomfort is more broad, generic, or difficult to pin down. It can be difficult to pinpoint exactly what problem or mix of disorders is producing the symptoms you’re experiencing at times. When an infection exists in the root canals of a tooth as well as the gum tissue surrounding it, this may be the situation.
In this case, the infection could have started in the pulp of the tooth, or it could have started in the gums. It’s spread from one site to another over time, and now it’s generating a jumble of symptoms that are difficult to decipher. Regardless of how the disease began, a thorough examination is required before treatment can begin in order to maximize your chances of saving the tooth.
Confusing Symptoms
Many people suffer mild or intermittent oral soreness from time to time. A stimulus like temperature (from hot or cold foods or beverages) or pressure can sometimes cause a more persistent pain (from biting down on something). The aching may appear to originate from a collection of teeth rather than a single tooth — or even from the sinus area above the back teeth.
These signs and symptoms can suggest a variety of dental disorders, including root canals and gum disease, and they should not be ignored. However, if you can ignore the intense pain, it will usually go away with time. However, the news isn’t all good: It usually indicates that the diseased tissue in your tooth’s pulp has died and the nerve is no longer functioning. That’s when the issue could grow more serious.
Where does the infection originate?
These signs and symptoms can indicate a number of dental problems, such as root canals and gum disease, and should not be overlooked. However, if you can ignore the excruciating discomfort, it will eventually fade away. The news isn’t all good, though: It usually means the unhealthy tissue in your tooth’s pulp has perished and the nerve has stopped working. That is when the problem may become more serious.
However, the illness could also spread through an entirely different route. In this situation, an infection that started in the gums (often caused by plaque accumulation) may have spread through small passages called accessory canals, which are found between the roots of a tooth or on the sides of the roots. The infection might then spread to the pulp of the tooth. It’s especially simpler for disease to spread if your teeth are cracked.
Treatment Methods
When a tooth is impacted by both root canals and gum disease, preserving the tooth can be difficult. This is when it’s crucial to know where the illness began: If the disease is largely a root-canal issue that has spread to the gums, the tooth’s prognosis is good if it is treated right away. However, if gum disease occurs first, the prognosis is frequently bad; by the time the infection spreads to the tooth, it’s probable that a significant amount of bone has already been destroyed, making the tooth’s long-term prognosis poor.
In either situation, the reason of the tooth discomfort must be identified and a treatment strategy devised. The sooner this occurs, the better: root canal and gum issues do not improve on their own.
Meet Your Award-Winning Dentists in Mission Viejo & Fullerton, CA








Our Dental Services
General Dentistry
Dental Implants
Emergency Care
Pediatric Dentistry
Oral Surgery
Orthodontics
The Proof is in our Patients

2 Convenient Locations
Our Fullerton, CA Office
1950 Sunny Crest Dr., Ste #1100
Fullerton, CA 92835
Working Hours
Our Mission Viejo, CA Office
24896 Chrisanta Drive, Suite #110
Mission Viejo, CA 92691







